
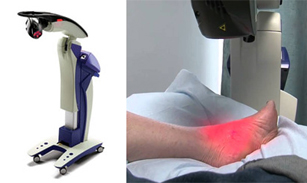
MLS, or Multiwave Locked System laser therapy, is an advanced and non-invasive medical technique that utilizes laser light to stimulate the body's natural healing processes. The therapy involves the use of dual wavelengths of light to penetrate tissues, reducing pain and inflammation while accelerating the healing of damaged cells. MLS laser therapy finds applications across various medical fields. It is often employed to address chronic and acute musculoskeletal conditions, such as arthritis, tendonitis, and sports-related injuries. The therapy works by improving blood flow to the affected area and promoting the production of endorphins, the body's natural painkillers. This leads to reduced pain, increased mobility, and enhanced tissue repair. In addition to pain management, MLS laser therapy is utilized in wound healing, post-operative recovery, and foot conditions. Its non-invasive nature and minimal side effects make it a valuable option for those seeking relief from various medical conditions. Understanding the definition and applications of MLS laser therapy sheds light on its significance in modern healthcare, offering an alternative approach to pain relief and healing. If you are interested in learning more about MLS laser therapy to treat your foot condition, it is suggested that you consult a podiatrist who can determine if this treatment method is right for you.
MLS Laser Therapy is a successful alternative for treating any pain you may be experiencing related to certain podiatric conditions. If you are interested in MLS Laser Therapy, consult with one of our podiatrists from Riznyk Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
MLS Laser Therapy
Multiwave Locked System (MLS) Laser Therapy is a patented, FDA-cleared technology that helps relieve pain and inflammation from a number of podiatric conditions, including:
MLS Laser Therapy is an ideal alternative to surgery and prescription medication, as it has no negative side effects and encourages accelerated healing. Among its many clinical benefits, MLS Laser Therapy also:
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
MLS Laser Therapy is an FDA-approved technology designed to treat various painful conditions. It is often sought out as a successful alternative to surgical treatment and prescription medication that may otherwise bring about negative side effects. During MLS Laser Therapy, light energy enters the damaged cells to stimulate intercellular activity, reducing pain in the affected area and accelerating the recovery process.
MLS Laser Therapy is used in podiatry to treat various conditions. These include heel pain, plantar fasciitis, sports injuries, wounds, Achilles tendonitis, arthritis, neuromas, neurological pain, musculoskeletal disorders, and sore muscles. Aside from the specific conditions MLS Laser Therapy treats, patients can also gain from the treatment’s general benefits. These benefits include a rapid relief of pain, the reduction of swelling caused by inflammation or bruising, faster healing, improved blood circulation, the reduction of scar tissue, and improved nerve function.
MLS Laser Therapy is a non-surgical treatment with no side effects. The treatment process is painless and typically takes a short amount of time to complete. Several treatments may be required depending on the specific condition.

Red feet in the elderly can be a symptom with a myriad of potential causes. One primary contributor is reduced circulation, a common age-related issue that compromises blood flow to the extremities. Chronic venous insufficiency, where weakened veins struggle to return blood to the heart, may result in redness in the feet due to pooling blood. In some cases, medications or medical conditions affecting blood vessels can contribute to this discoloration. Additionally, inflammatory conditions like arthritis or infections might manifest as redness in the feet. Diabetic complications, particularly peripheral artery disease, may also lead to diminished blood supply and red discoloration. A podiatrist needs to conduct a thorough assessment to accurately diagnose and address the root causes of red feet in the elderly. If you or someone you know has this foot condition, it is suggested that you visit a podiatrist who can offer appropriate treatment options.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
While proper foot care is important for everybody, senior citizens have the tendency to be more susceptible to certain foot conditions. The elderly should therefore be well informed about any problems that may arise and about what they can do to properly avoid or treat them.
Some of the most common foot problems seniors are susceptible to include foot ulcers, ingrown toenails, fallen arches, and fungal nails. A foot ulcer is an open sore on the foot and can be a result of diabetes and decreased sensation in the feet. An ingrown toenail is defined as when the nail grows into the side of the toe. Fallen arches are indicated by the instep of the foot collapsing. A fungal nails is a condition that results in deformed and discolored toenails.
In order to avoid these conditions it is recommended that the feet be inspected by the patient on a regular basis. If these inspections are carried out routinely, there is a good likelihood that problems can be identified before they become severe, or can even be avoided altogether. If any abnormality is discovered, it is important that the individual consult a podiatrist for diagnosis and information on treatment options.
Proper foot hygiene is also important. Making sure that you always have clean, dry socks on can be a major deterrent to many different problems including bacterial infections, foot odor, and certain types of fungus. Wet feet are a major cause of many of these problems. If your socks get wet, it is important to change them. Walking around in wet socks may not only lead to various infections, but can irritate the skin and result in a number of various complications. Clean, dry feet are less likely to be affected by fungal and other infections.
As people age, the fat present on your feet begins to deteriorate. The protective nature of this fat keeps the feet healthy by providing a barrier between your bones and the ground. This also aids in giving the skin on the feet a certain amount of elasticity. This is one factor that causes elderly people to develop some serious foot issues. Foot moisturizers can be helpful to avoid certain problems associated with this. However, water-based moisturizers do not work as well for elderly people as they do for the young. Instead, it is more effective to use an emollient instead. An emollient is effective because it binds the water in the foot, keeping it from becoming absorbed too readily which will result in dry skin. Emollients also have a special property called occlusion, which provides a layer of oil on the skin. This layer prevents the foot from drying up and can be very effective in treating dry skin disorders. If you can keep the skin on your feet healthy, this will substantially reduce the number of foot problems you will encounter in old age.
Proper footwear is another way to keep feet healthy. Shoes that fit well and provide proper support help prevent ingrown toenails and fallen arches.
Certain medical conditions such as diabetes or poor blood circulation increase the risk for foot issues. For individuals with any of these conditions it is extremely important to conduct regular foot inspections to make sure that there are no sores or infections present.
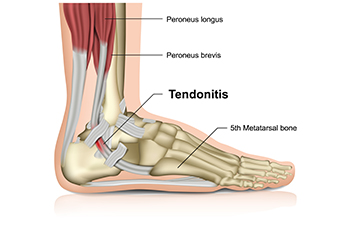
Achilles tendonitis, a common woe for runners, arises from inflammation in the strong tendon that connects the calf muscles to the heel bone. Typically linked to the runner's trifecta of too much, too fast, and too soon, recognizing symptoms of Achilles tendonitis is vital for timely intervention. These symptoms include initial stiffness that dissipates with warming up, in addition to pain and swelling near the heel. The runner may experience limited ankle flexibility during physical activities, and notice redness along the tendon. Other symptoms can include a distinct burning sensation, palpable scar tissue lumps, and an audible cracking or popping sound during ankle movement. Runners, constantly pushing their limits, are particularly prone to Achilles tendon injuries due to the repetitive stress involved in each stride. Speed and uphill training can increase the strain on the tendon. This can lead to overworking, tightening, and inflammation, which may result in Achilles tendonitis. If you are experiencing symptoms of Achilles tendonitis, it is suggested that you schedule an appointment with a podiatrist for a complete examination and treatment suggestions.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.

Foot blisters are tiny fluid-filled sacs that form on the skin. They may seem inconspicuous but can be surprisingly uncomfortable, often arising from a combination of factors. Friction stands as a primary cause, especially when ill-fitting footwear or repetitive motion induces rubbing against the skin. Moisture and heat exacerbate the risk, as sweaty or damp conditions soften the skin, making it more prone to friction-related blisters. Additionally, poorly managed moisture, whether from excessive sweating or wet environments, creates an ideal environment for blisters. The symptoms of foot blisters include localized pain, tenderness, and a distinct swelling filled with clear fluid. The affected area may become red, and in more severe cases, the blister may rupture, leading to an open wound susceptible to infection. If you repeatedly develop foot blisters, it is suggested that you confer with a podiatrist who can offer effective relief and prevention methods.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact one of our podiatrists of Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.

Cracked heels, a common foot ailment, manifest as fissures or splits in the skin around the heel area. The primary cause of this condition lies in the lack of moisture, leading to dry and hardened skin. Prolonged standing or walking on hard surfaces can exacerbate the problem, as the pressure on the feet intensifies. Obesity is another contributing factor, as excess weight puts additional strain on the feet, fostering the development of cracks. In some cases, underlying medical conditions such as diabetes or hypothyroidism may contribute to the dryness of the skin, increasing the risk of cracked heels. Lack of proper foot care, including infrequent moisturizing and neglecting to exfoliate dead skin, further amplifies the susceptibility to cracked heels. Understanding these causes is pivotal for adopting preventive measures and a comprehensive foot care routine, ensuring the maintenance of soft, healthy heels. If you have developed cracked heels, it is suggested that you visit a podiatrist who can offer you correct treatment and prevention techniques.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.