
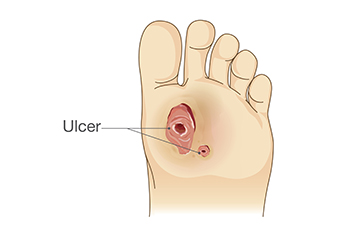
Diabetic foot ulcers are serious wounds that develop on the feet of individuals with diabetes, primarily due to nerve damage and poor circulation. Common causes include prolonged pressure, injury, or infection, which can occur when blood sugar levels are poorly managed. Symptoms typically include red or swollen areas, open sores, and sometimes drainage or a foul odor. If left untreated, these ulcers can lead to severe infections and even amputation. Treatment involves wound care, proper footwear, and controlling blood sugar levels. A podiatrist plays a key role in managing diabetic foot ulcers, offering specialized assessments, debridement of the wound, and creating a tailored care plan. They can also provide advice on footwear to prevent further injury. If you or a loved one is experiencing symptoms of a diabetic foot ulcer, it is suggested you make an appointment with a podiatrist. Early intervention can help prevent complications and promote healing.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.

Morton’s neuroma, or interdigital neuroma, is a painful condition caused by the thickening of tissue surrounding one of the nerves in the midfoot, often between the third and fourth toes. This irritation results from nerve compression, frequently due to repetitive stress or pressure from wearing tight or high-heeled shoes. The condition can feel like a sharp, burning pain in the ball of the foot, often radiating to the toes. Some patients describe it as feeling as though they are standing on a pebble, or having a clicking sensation. Risk factors include high-impact activities like running, foot deformities such as bunions or flat feet, and poor footwear choices. Diagnosis often involves a physical exam, an ultrasound, or an MRI scan. Treatment ranges from modifying footwear and orthotics to corticosteroid injections or, in severe cases, surgical removal of the affected nerve tissue. If you have this odd and painful sensation in your foot, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Riznyk Podiatry. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.

Acute and chronic sports injuries are common among athletes and active individuals. Acute injuries occur suddenly during physical activity, often due to falls, collisions, or improper technique. Common examples include sprains, fractures, and muscle strains. Symptoms typically involve immediate pain, swelling, and an inability to use the affected area. In contrast, chronic injuries develop gradually over time, often due to repetitive stress on muscles and joints. Conditions such as tendinitis, bursitis, and stress fractures are common. Symptoms may include persistent pain, stiffness, and swelling that worsen with activity. Treatment for acute injuries usually includes rest and elevation. Chronic injuries often require a more comprehensive approach, including targeted exercises, activity modification, and sometimes medications or injections. If you are experiencing persistent pain or difficulty due to a sports injury, it is suggested that you schedule an appointment with a podiatrist for an accurate diagnosis and effective treatment tailored to your needs.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with one of our podiatrists from Riznyk Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.

Diabetic patients with foot ulcers can experience significantly reduced quality of life due to chronic pain, limited mobility, and the risk of serious complications like infection or amputation. These ulcers, often caused by poor circulation and nerve damage, can make everyday activities difficult and may lead to prolonged hospital stays or social isolation. The emotional toll, including stress and anxiety, further impacts their overall well-being. Managing foot ulcers in diabetic patients requires a comprehensive approach. Regular foot exams by a podiatrist, proper wound care, and the use of custom orthotics or footwear can help reduce pressure and promote healing. Blood sugar control is critical in preventing further damage. In more severe cases, advanced treatments like hyperbaric oxygen therapy or surgery may be needed. If you suffer from diabetic foot ulcers, it is strongly suggested that you include a podiatrist on your team of healthcare providers to improve functioning. Education on daily foot care, combined with early intervention, can help prevent ulcers and improve your well-being.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Riznyk Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.

Orthotic insoles can be helpful for people with mild leg length discrepancies, a condition where one leg is slightly shorter than the other. This difference, even if small, can affect how a person walks, causing discomfort or pain. Orthotic insoles are designed to help balance the body and improve how the legs and feet move together. Research shows that using custom orthotics can improve gait symmetry, meaning the walking pattern becomes more even and natural. By leveling out the legs, insoles help reduce immediate pain and discomfort caused by uneven pressure on the feet, knees, hips, and lower back. If you are experiencing foot pain and you know your legs are slightly different lengths, it is suggested that you schedule an appointment with a podiatrist who can provide appropriate treatment, which may include custom orthotics.
If you are having discomfort in your feet and would like to try orthotics, contact one of our podiatrists from Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.