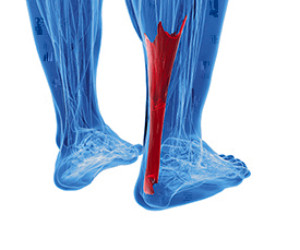
There is no mistaking an Achilles tendon injury when it occurs. This large tendon, located at the back of the calf, connects the calf muscles to the heel bone. It is responsible for pointing and flexing the feet, which is necessary in completing daily activities. An injury can happen from increasing running mileage and speed too quickly, which can cause severe pain and discomfort. Patients who have experienced this type of injury find it difficult to walk and are unable to bend their ankle. Mild relief may be found by taking anti-inflammatory medicine, and it may help to stretch the calves. Effective prevention techniques for an Achilles tendon injury includes strengthening the feet and calves as often as possible, which can help to ease the loading force on the tendon. This is accomplished by standing on a step, and lowering the heels one at a time, until a stretch is felt. An Achilles tendon injury often needs immediate attention, and it is strongly suggested that you confer with a podiatrist as quickly as possible who can guide you toward the correct treatment techniques.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
Plantar fasciitis occurs when the fibrous ligament that stretches from the heel to the toes on the bottom of the foot, called the plantar fascia, becomes strained or even torn. The plantar fascia is prone to injury as it bears the body’s weight while walking and jumping. People who stand at work or overly stress the plantar fascia doing excessive repetitive movements during athletics are more at risk for developing this condition, which is the most common form of heel pain. Other risk factors include having flat feet or high arches, as well as wearing improper shoes or running on hard surfaces. Type 2 diabetes and certain rheumatic disorders are also risk factors. A podiatrist can often diagnose plantar fasciitis with just a physical exam, however, X-rays may also be used to rule out other possible conditions. If you believe you have developed plantar fasciitis, make an appointment with a podiatrist as soon as possible to be properly diagnosed and treated.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
 The medical term for the foot condition that is known as an ingrown toenail is referred to as onychocryptosis. It occurs when the toenail grows into the skin and can cause severe pain and discomfort. It can happen as a result of trimming the toenails incorrectly, or from wearing shoes that do not fit properly. Noticeable symptoms that patients can see include redness and swelling, and there may be drainage from the injured nail. The most common toe that is affected is the big toe, and it can cause difficulty in walking. Mild relief may be found when the toe is soaked in warm water, and this may help to soften the skin. If you have an ingrown toenail, it is strongly advised that you are under the care of a podiatrist who can properly treat this condition.
The medical term for the foot condition that is known as an ingrown toenail is referred to as onychocryptosis. It occurs when the toenail grows into the skin and can cause severe pain and discomfort. It can happen as a result of trimming the toenails incorrectly, or from wearing shoes that do not fit properly. Noticeable symptoms that patients can see include redness and swelling, and there may be drainage from the injured nail. The most common toe that is affected is the big toe, and it can cause difficulty in walking. Mild relief may be found when the toe is soaked in warm water, and this may help to soften the skin. If you have an ingrown toenail, it is strongly advised that you are under the care of a podiatrist who can properly treat this condition.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact one of our podiatrists of Riznyk Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
 Many older people are at an increased risk of falling. It is believed that one-third of people over 65, and half of people over 80, fall at least once a year. Common factors that contribute to the likelihood of falling are impaired vision, loss of balance, dizziness, muscle weakness, and low blood pressure. Also, diabetic neuropathy (which causes numbness in the feet), slick or highly polished floors (especially in the bathroom), loose rugs, poor lighting, and pathways blocked with furniture may risks. Actions like slipping on a ladder or step stool, reaching for something too high, or going down stairs may cause falls. One good way to prevent a fall is by paying attention to your surroundings. Here are some suggestions to help lessen the risk: Use non-slip mats in the bathroom, and wear shoes or slippers with non-skid soles; get help moving heavy items and carrying awkward objects; make sure hallways have adequate lighting; use a cane or walker if balance is an issue; and remove throw rugs and loose carpeting. If you are at risk of falling, it may be wise to see a podiatrist for guidance in proper footwear and an examination to make sure your feet are not part of the problem.
Many older people are at an increased risk of falling. It is believed that one-third of people over 65, and half of people over 80, fall at least once a year. Common factors that contribute to the likelihood of falling are impaired vision, loss of balance, dizziness, muscle weakness, and low blood pressure. Also, diabetic neuropathy (which causes numbness in the feet), slick or highly polished floors (especially in the bathroom), loose rugs, poor lighting, and pathways blocked with furniture may risks. Actions like slipping on a ladder or step stool, reaching for something too high, or going down stairs may cause falls. One good way to prevent a fall is by paying attention to your surroundings. Here are some suggestions to help lessen the risk: Use non-slip mats in the bathroom, and wear shoes or slippers with non-skid soles; get help moving heavy items and carrying awkward objects; make sure hallways have adequate lighting; use a cane or walker if balance is an issue; and remove throw rugs and loose carpeting. If you are at risk of falling, it may be wise to see a podiatrist for guidance in proper footwear and an examination to make sure your feet are not part of the problem.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from Riznyk Podiatry. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Orchard Park, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.